Introduction
In multiple myeloma (MM) patients older than 65, the value of consolidation with autologous hematopoietic stem cell transplantation (auto-SCT) is not well defined. This is generally a population not represented in the pivotal clinical trials on which routine clinical practice is based. Even though the treatment of MM in older patients has improved in recent years, their survival is shortened, and most do not reach a second line. However, there are data supporting auto-SCT in this population with low associated mortality not related to relapse (NRM). TriNetX is a federated global health research platform that provides researchers with access to electronic medical records from healthcare organizations to conduct research studies. The aim of our study is to evaluate the safety and efficacy of auto-SCT in patients older than 65 years with MM with in a large population of world real life data.
Methods
We have analyzed the cohort of patients from our center (H12O) who have received an auto-SCT from January 2014 to March 2023. We defined two cohorts: Cohort 1, patients with > 65 years at the time of transplantation (n=59 patients) and Cohort 2, <= 65y (n=213 patients).
Data from the last 20 years of the TriNetX platform of 48 centers have been used. Cohort 1, patients with > 65 years included n=6,876 patients; and Cohort 2, <= 65y included n=11,046 patients. Propensity score matching (PSM) was performed on 8 characteristics: in the Demographics category patients were matched on female or male. In the diagnosis category patients were matched on Hypertensive diseases, Ischemic heart diseases, Chronic kidney disease, Diabetes mellitus, Diseases of liver, Chronic lower respiratory diseases characteristic.
Results
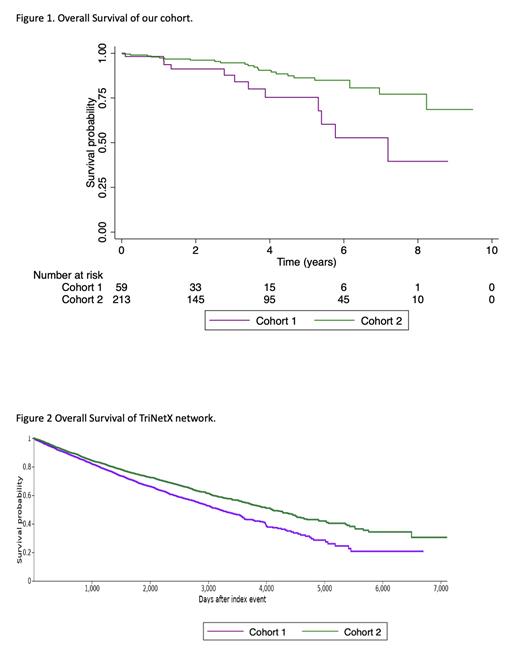
In the H12O cohort of patients, the median age was 68 (66-74) in >65 y patients and 57 (28-65) in <65 y patients. The older population presented greater comorbidity measured with the Charlson Index (p=0.001) and a history of another neoplasm (p=0.009). There were no differences in the type of MM, ISS disease stage, type of conditioning, pre-transplant response, induction treatment, number of lines or previous transplants. With a median follow-up of 3.4 years the probability of survival was 39.6 % in Cohort 1 and 68.6 % in Cohort 2 (HR, 2.69 95% CI, 1.34 to 5.44, p=0.004) (Figure 1). PFS at the end of follow-up was similar in both groups: 35%.5 in Cohort 1 and 42.9 % in Cohort 2 (HR, 1.36 95% CI, 0.79 to 2.32, p=0.26).
The older population required admission to the Intensive Care Unit more frequently (20.3% vs 10,4%, p=0.041), without an associated increase in NRM (1.7 % vs 1.4 %, p=0.871). We found no significant differences in the recovery time of neutrophils or platelets, blood component transfusion, and transplant complications, and short-term survival was similar between both cohorts.
At TriNetX database, after the PSM, the final population was 5,820 patients in each cohort. Cohort 1 with a mean age (+-SD) of 69.7 (3) years and Cohort 2 of 55.6 (7.8) years. The rest of the variables were balanced. The probability of survival at the end of follow-up was 20.8 % in Cohort 1 and 30.5 % in Cohort 2 (HR, 1.29, 95% CI, 1.20 to 1.39, p<0.001) (Figure 2). The relative risk of any transplant complication was significantly lower in Cohort 1 vs. Cohort 2 (0.82, 95 % CI, 0.73 to 0.93). As well as in the other cohort short-term survival was similar between both cohorts.
Conclusion
We have found that ASCT in MM patients older than 65 years have the similar NRM, PFS and performance. However, the long-term outcome of these elderly patients is dismal, probably due to the limited options of rescue after the relapse and the impact of the age. This large-scale study shows that ASCT in MM patient, between 65 and 70 years, had similar results.
Disclosures
Ayala:Novartis: Consultancy, Speakers Bureau; Incyte: Consultancy; Astellas, BMS: Speakers Bureau.